The following is the third in a series of interviews with a nurse who works in a hospital on the outskirts of Toronto, Ontario. She has provided sufficient evidence, and links to public records, to satisfy me that she is indeed a registered nurse working for over a decade in multiple Canadian hospitals, serving both in the emergency room and intensive care unit.
To protect her identity, position and family, details about her and her place of work have been changed or omitted, without altering her message. In this interview, we focus on her frontline perspective of the current situation in her hospital during a supposed third wave of COVID-19 and related variants.
JOHN: How would you describe the current situation in the hospitals that you work in?
NURSE ANDREA: It seems like there might be an actual surge of COVID patients. Not a catastrophe, and we’ll be fine, but urban hospitals are seeing more of a “wave” of acute respiratory illness now compared to any time in the last year. This puts pressure on the Intensive Care Unit (ICU) and creates a spillover effect of sick people into the other inpatient acute care units.
JOHN: So after a year of working far below capacity, we are finally seeing hospitals starting to get busy again?
NURSE ANDREA: The first wave was barely a ripple last spring. The second wave during fall and winter put some pressure on the ICUs, akin to typical flu season. The recent third wave has resulted in some ICUs getting maxed out with ventilated patients. Some non-ventilated patients who might typically require ICU are being managed on regular hospital wards.
JOHN: Do you think people are sick with the so-called “variants?”
NURSE ANDREA: They say it’s the mutant strains. Certain areas are seeing a wave of endemic illness and it fits with the pandemic narrative we’ve been talking about all year. My hospital has received some intubated patients from the hotspots in Toronto.
JOHN: Is it normal for you to see intubated patients being transferred to your hospital?
NURSE ANDREA: It is not typical to have critically ill, ventilated patients transferred to my hospital from higher-level centres. But it’s not unheard of. I’m not sure why it’s happening now — other than there is some truth to the official narrative that a novel viral infection is sweeping through populations, like in Toronto and Peel, where it’s most likely to be transmitted in settings like industrial warehouses and more densely packed urban and suburban dwellings.
JOHN: Are you seeing more younger patients with flu-like symptoms?
NURSE ANDREA: Anecdotally, my experience does correspond with the claims that younger people are presenting with respiratory trouble. Typically ethnic minority, late middle-aged men in their 50s and 60s. Usually, a whole family has gotten sick but the father is hit the worst. My observation is consistent with the macro data across the world as shared by the CDC.
JOHN: Why do you think people are suddenly getting sicker?
NURSE ANDREA: I ask these patients how they believe the virus entered their house to infect everyone, and most claim to have no idea. They claim they’ve been doing everything they were told to do by the health authorities, like masking and social distancing.
Anecdotally, a lot of descendants from Africa (blacks) and South Asians (from Pakistan and India) are getting very sick. This possibly relates to their special vulnerability to vitamin D deficiency living in northern climates and high rates of underlying disease like diabetes and high blood pressure.
My theory is these people have been made extra vulnerable because of the depression and forced sedentarism of lockdown. The forced humid microbial traps on their faces we call masks likely don’t help either.
JOHN: Is this surge all serious respiratory cases?
NURSE ANDREA: Not at all. For months, emergency was vastly underutilized but now I notice people come to the hospital for minor complaints. So this is adding pressure to the hospital system. In some cases, it seems like people are bored and looking for something to do, so they come to the hospital for a pulled muscle or stubbed toe. In many cases, their family doctor or nurse practitioner is only seeing people over a computer screen so they are forced into a crowded emergency room to get actual healthcare.
I’m not sure why so many family doctors are not seeing patients in real life and forcing their patients to go to the emergency room for minor complaints they would typically deal with in their office. I know this sounds harsh and judgemental, but I think it’s a combination of laziness, cowardice, and obsequious deference to public health authority telling them to deliver healthcare over a screen or telephone.
JOHN: How, exactly would you describe the ICU situation at the moment?
NURSE ANDREA: Busy. Lots of staffing demands. But ICU capacity is a lot more flexible than we think.
There are hard limits to capacity, such as the number of beds, ventilators, and trained staff. However, frontline clinicians are highly adaptable to crises, and not every clinician treats the same situation in the same way. Consider the decision to intubate a patient. Some doctors like to intubate early, while others will essentially wait until the patient is crashing. The doctor who delays intubation may discover that the patient didn’t need intubating after all. So in some cases, resource limitation might be a good thing.
JOHN: How would you explain such radically different approaches to the use of a life-threatening procedure?
NURSE ANDREA: One of the drivers of early intubation can be the anxiety level of the staff. But one thing we’ve learned with COVID is that many patients survive without being intubated. I’ve seen many patients that would have been guaranteed a bed in ICU —based on the same clinical parameters used in the past — nowadays do fine with a little patience from the staff and rapid deployment of other therapies that work.
As an aside, I think one of the reasons some patients deteriorate in hospital and require ICU is due to the lack of family support.
JOHN: How many of these ICU patients have genuine severe respiratory disorder?
NURSE ANDREA: In emergency, I am seeing people present with rapid breathing and low oxygen saturation. These symptoms correspond with X-rays showing diffuse inflammatory change in the lungs. The proverbial “ground glass” picture you’ve probably heard about in the media.
JOHN: So there is definitely a rise in cases of patients with COVID symptoms?
NURSE ANDREA: Yes, there’s definitely more pressure on the acute care hospital system. I haven’t seen this for the whole year. It’s interesting how this is happening now.
JOHN: Of course, according to a January 22, 2020 CBC News article, hospital gridlock — with beds in hallways and conference rooms — had become a routine reality in many of Ontario’s hospitals long before COVID-19.
NURSE ANDREA: Yes, we’ve had a year to meaningfully change the system so we wouldn’t have to resort to lockdown. But it’s like we’ve learned nothing. It’s an outrage, in my opinion. It’s almost like lockdown is the desired outcome, as fixing the so-called hospital capacity problem would make lockdown unnecessary. That’s assuming lockdowns work toward the purported end of mitigating viral illness, which they don’t, hence we are seeing this surge despite living in one of the most heavily locked down jurisdictions in the world.
JOHN: Do you think that these symptoms are being caused by a virus?
NURSE ANDREA: I have no other explanation for what’s causing these symptoms other than a virus. Granted, since the onset of COVID, I’ve become more open to alternative explanations about the nature of what we call “viral illness” because so much about what’s going on does not add up.
JOHN: What’s not adding up?
NURSE ANDREA: For example, I’ve spent the majority of my adult life immersed in illness in hospitals, presumably surrounded by viral pathogens. How is it possible then that I hardly ever get sick? In the last year I’ve been exposed to tons of people with a virus that is supposedly so transmissible we need to shut down society, but I have not gotten sick. Even under conditions where COVID is most highly transmissible, such as with aerosol-generating procedures like intubation and high-flow oxygen therapies, myself and all my colleagues doing the same are still standing, unscathed. PPE can’t be the only explanation because we know the virus passes right through and around it.
I spoke to one nurse who told me she secretly and deliberately goes into the rooms of highly infectious COVID patients, removes her mask and takes deep breaths in an attempt to develop her own immunity, and has never shown any symptoms. Personally, I wear the least PPE possible.
Up until this last year, I never wore a mask in the presence of patients with viral-induced acute respiratory illness; but I never acquired illness at a rate higher than people who are not exposed to viruses in the same way.
JOHN: Why do you think the big city hospitals are seeing an increase in patients, while rural communities are not?
NURSE ANDREA: It makes sense if you follow the logic of viral spread being greater among greater concentrations of people. You have more ethnic minorities and people at the lower end of the socio-economic ladder whom we know are more affected by COVID, as we discussed earlier.
JOHN: Would you say that all of the patients currently in ICU actually require ICU?
NURSE ANDREA: Currently, I would say yes, for the most part. But in normal times, ICU routinely has non-ICU patients. Sometimes this is due to a lack of beds to discharge the patients, too. Other times, this is because the ICU doctor doesn’t get paid as much if there are no patients in the ICU. There has always been structural incentives to keep the ICU near capacity.
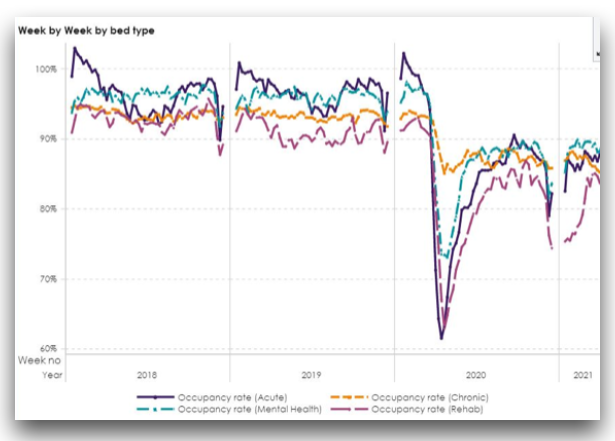
For years, most hospitals run at 90-110% capacity. Look at the peak in the 2018 flu season. Look at January 2020. Way higher than anything during COVID, where the hospital has been sitting at 60-80% capacity throughout the last year.
JOHN: Can you talk more about how limited ICU capacity is in an Ontario hospital?
NURSE ANDREA: I think it’s important to emphasize that, at baseline, critical care capacity is always on the cusp of overwhelm. In my first interview, I mentioned how a ten-bed ICU could have nine patients, hence being at 90% capacity. Discharging two patients would bring it down to 70% capacity. Conversely, a marginal shift in demand of three patients could send an ICU from 70% capacity, essentially underwhelmed, to being completely overwhelmed in a matter of minutes.
Under normal circumstances, all it would take is two simultaneous code-blue events in a hospital, or a multiple casualty accident near the hospital to cause overwhelm.
Imagine a house near the hospital where multiple people overdose at the same time on opioids or alcohol, all needing to be rushed to the hospital for critical care services. All these scenarios, and more, represent a risk for hospital overwhelm. If they do happen, frontline clinicians rapidly adjust and adapt to accommodate these situations.
JOHN: Why is critical care capacity as low as it is considering the chronic risk of overwhelm?
NURSE ANDREA: The reason is that it is extremely expensive to maintain critical care capacity. The government deliberately limits the number of critical care beds as de facto rationing. The more you make critical care available, the more it gets used. While the supply of critically ill patients creates demand for critical care services, the supply of critical care services can also create the demand for critical care services. A healthcare administrator once told me that when it comes to hospitals, “if you build it, they will come.”
Ask any ICU nurse and they will tell you: the difference between an overwhelmed ICU and one that is under control can be determined by the particular doctor working that week. Some doctors will inherit a bunch of empty beds from the previous doctor and rapidly start filling up the ICU with non-ICU patients while the nurses scratch their heads saying, “Does this patient need to be in ICU? What if there’s a code blue and we need this bed for that patient?”
Nursing organizations are also to blame for their rent-seeking behaviour. The Ontario Nurse’s Association (our union) has lobbied hard to limit nurse-to-patient ratios in Ontario ICUs to among the lowest in North America. They argue it’s for patient safety, but it’s also a means of artificially limiting critical care labour capacity to leverage for more union-dues paying RNs[,] when there’s no reason an unlicensed caregiver can’t provide delegated help. The union and Registered Nurses Association of Ontario (RNAO) has lobbied to prohibit unregulated support workers from helping in the ICU.
JOHN: Are you seeing any correlation between the increase in hospitalization and adverse reactions to the COVID-19 vaccine?
NURSE ANDREA: Yesterday, a patient came in by ambulance who lost consciousness five minutes after receiving the COVID-19 vaccination. The bloodwork showed a very low white blood cell count. I was working with that same doctor referenced in my last interview. The doc dismissed any relationship between the low blood count and the vax. He said: “Bah, it’s just incidental!”
JOHN: I would understand if it was five days later, claiming the vaccination was “incidental” — but to lose consciousness after only five minutes? How could a doctor exercise such cognitive dissonance?
NURSE ANDREA: Like I said in a previous interview, clinicians are biased toward the efficacy of our interventions. I would go further to say we are even blinded by lust over the supremacy and efficacy of our interventions.
The whole idea of forced vaccination, vaccine passports, and all this stuff is not new or unique. It’s deeply embedded in the medical tradition. In many ways, I think the institution of medicine as such, right down to the way many doctors practice, is fundamentally at war with the concept of individual autonomy.
JOHN: Thank you very much for providing this frontline perspective of the situation in the “epicentre” of Ontario’s supposed corona mutant variant pandemic.
NURSE ANDREA: I sincerely thank you again for giving me this platform to share my thoughts and perspective. The truth will win out in the end.